Hypospadias
Hypospadias
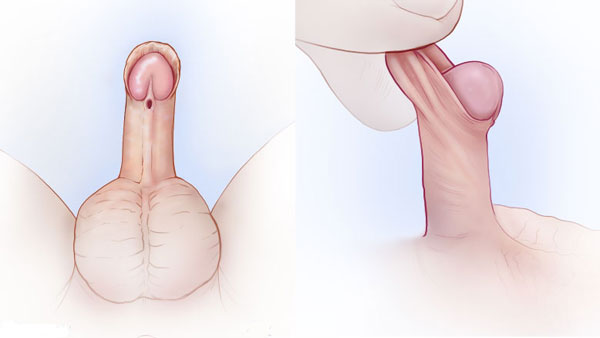
It is a urethral developmental defect in children in which the opening of the urethra lies on the underside of the penis rather than at the tip.
Types
- Glandular hypospadias – commonest types
- Coronal hypospadias – the meatus is located at the intersection of the bottom of the glans and the body of the penis.
- Penile and penoscrotal hypospadias — the aperture is located on the underside of the penile shaft.
- Perineal hypospadias occurs when the scrotum is divided and the urethra opens between the two halves.
What are the symptoms and indicators of hypospadias?
Among the signs and symptoms are:
- The foreskin and penis have an unusual look (may not be symmetrical or appear disfigured)
- Abnormal direction of urine stream (may come from the underside of the penis, or wherever the urethra exits the penis)
- A downward curve to the penis
How to diagnose hypospadias?
Because hypospadias is easily visible, it is frequently detected shortly after delivery during your child’s initial physical examination.
Although hypospadias is not an emergency, your child should consult a pediatric urologist as soon as possible after being diagnosed.
Hypospadias Degree
- In around 50–75 percent of instances, the urethral meatus opens on the bottom of the glans penis; this is classified as first-degree hypospadias.
- Second-degree urethral opening (when the urethra opens on the shaft) and
- Third-degree urethral openings (when the urethra opens on the perineum) occur in up to 20% and 30% of cases, respectively.
The more severe degrees are more likely to be linked with chordee, a condition in which the phallus is still attached to the perineum or is tethered downwards by connective tissue, or with undescended testicles (cryptorchidism).
Treatment for hypospadias
Except for the orientation of the urine stream, first-degree hypospadias is essentially an aesthetic deformity with minimal functional impact. If left untreated, second or third-degree hypospadias may make urination difficult, necessitating sitting, inhibiting transport of sperm into the vagina (potentially causing reproductive issues), or interfering with erections.
- Surgical correction of first and second-degree hypospadias is virtually always effective in a single treatment, which is generally done by a pediatric urologist within the first year of life.
- When the hypospadias is third degree or there are other birth abnormalities present, such as chordee or cryptorchidism, the optimum therapy might be a more difficult option. To diagnose intersex disorders or hormone deficits, a karyotype and endocrine examination should be conducted. If the penis is small, testosterone or human chorionic gonadotropin (hCG) injections may be administered prior to surgery to increase it.
- A Pediatric Urologist may need to do numerous operations including mucosal grafting to treat severe hypospadias. Circumcision should be avoided before repair because preputial skin is often utilized for grafting. Surgery causes poor outcomes in a minority of individuals with severe hypospadias, such as scarring, curvature, or the creation of urethral fistulas, diverticula, or strictures. A fistula is an abnormal opening through the skin along the course of the urethra and can result in urinary leakage or an abnormal stream. A diverticulum is a “outpocketing” of the urethral lining that interferes with urine flow and may cause post-urination leaks. A stricture is a significant constriction of the urethra that prevents flow. (check these )
- Reduced complication rates have been recorded in recent years from facilities with the greatest expertise (e.g., fistula rates < 5%), and surgical correction is routinely undertaken for the vast majority of infants with hypospadias.
For more information & consultation on Hypospadias, Get in touch with Dr. Adwait Prakash a Pediatric Surgeon in Indore. will help you out in understanding your problem and guide you through every stage of your treatment.
To book your appointment Call: 8889588832.
